Abstract
Introduction: Thromboelastography (TEG) is used to rapidly assess global coagulation status. A few studies in the literature have explored a possible role for TEG in anticoagulant monitoring, with conflicting observations. We wondered if TEG might be used adjunctively with traditional markers of anticoagulation as a measure of anticoagulant efficacy. We hypothesized that some of these variations might be due to changes in certain coagulation factor levels.
Methods: Blood samples were collected from patients on therapeutic doses of warfarin, low molecular weight heparin (LMWH, enoxaparin or dalteparin), or an anti-Xa direct oral anticoagulant (DOAC, apixaban or rivaroxaban) due to a history of thrombosis. TEG was performed on all samples with and without addition of heparinase; R time, K time, alpha-angle, maximum amplitude, and percent of clot lysis after 30 minutes were measured. Standard anticoagulation parameters were obtained at the same time as TEG values [prothrombin time (PT) and activated partial prothrombin time (PTT) for warfarin- and DOAC-treated patients; anti-Xa level for LMWH-treated patients]. For each patient, pertinent medical history was recorded including: age, medical comorbidities, and thrombotic history. Von Willebrand factor (vWF) antigen level, factor VIII (fVIII) activity, anti-Xa, and R time were examined in a follow-up cohort of enoxaparin-treated patients. Correlation between TEG and anticoagulation parameters was analyzed using Spearman correlation coefficient (r).
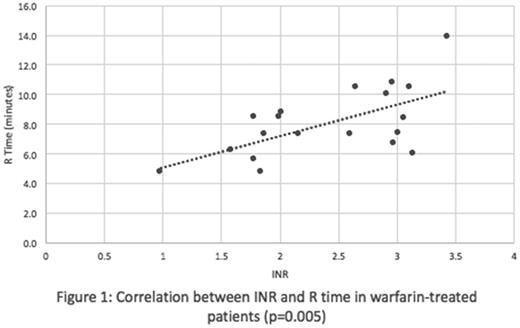
Results: Forty-six patients participated in this study. Median age was 52 years (range, 20-83). The most common indication for anticoagulation was deep venous thrombosis or pulmonary embolism ( N = 33); 5 subjects had active cancer at the time of anticoagulation testing (all on LMWH). Among warfarin-treated patients ( N = 19), INR was significantly correlated with R time (Figure 1, p=0.005), with 4 patients demonstrating a prolonged R time of over 10 min. Among patients on LMWH (enoxaparin, N = 13; dalteparin, N = 1), 5 had a prolonged R time, but there was no correlation between anti-Xa level and R time, R time ratio or R time difference with or without heparinase, or any other measured TEG parameter when analyzing all LMWH patients or only enoxaparin-treated patients as a function of total daily enoxaparin dose. Among DOAC patients (apixaban, N = 6; rivaroxaban, N = 8), R time was not elevated in any of the samples, but there was a significant correlation between PTT and R time (p=0.006). Four study patients had recurrent thrombotic events (1 with antithrombin deficiency, chronic liver disease, and bowel resection, on warfarin; 1 with May-Thurner syndrome, on LMWH; 2 with metastatic cancer and Trousseau's syndrome, also on LMWH) in spite of therapeutic INR or anti-Xa levels; these patients were all found to have normal R times on TEG. In a follow-up analysis of 8 enoxaparin-treated patients, 6 had normal and 2 had prolonged R times. All 6 with normal R times had elevations in vWF and/or fVIII, while the 2 with prolonged R times had normal levels of vWF and fVIII.
Conclusion:TEG R time is significantly correlated with INR in patients on warfarin. TEG R time is also correlated with PTT in patients on DOACs. For both DOACs and warfarin, TEG could be useful in rapidly assessing the coagulation status of patients who present with emergent bleeding and may benefit from reversal agents. In patients on LMWH, TEG R time is affected by circulating levels of vWF and fVIII. For select patients on LMWH, TEG may be helpful as an adjunctive measure of anticoagulant activity in cases where anti-Xa monitoring may not be accurate.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal